多管齊下降低血糖,臨床療效卓爾不凡。
2型糖尿病(T2DM)發病率逐年攀升,其引起心血管併發症所造成的危害與負擔日益嚴峻。而作為全球糖尿病防控的核心藥物,二甲雙胍的臨床應用也隨之愈發普遍。因此,對心血管專科醫生而言,了解並掌握二甲雙胍的作用機制及臨床療效,可以更好地管理合併心血管併發症的糖尿病患者。
上一期,我們已經了解了《二甲雙胍臨床應用專家共識(2018版)》中「二甲雙胍的臨床地位與使用時機」(二甲雙胍的臨床地位與使用時機,一文教你get!丨專家共識解讀第一篇),今天就一起來學習「二甲雙胍的作用機制及臨床療效」吧!
1多種武器齊上陣,360°降糖不留死角二甲雙胍作用途徑豐富,以多路並進的方式全方位、協同降低血糖,逐個擊破高血糖防線。
其主要降糖機制為:
-
作用於肝臟,抑製糖異生,減少肝糖輸出[1];
-
作用於外周組織(肌肉、脂肪),改善肌肉甘糖合成,降低遊離脂肪酸,提高胰島素敏感性,增加對葡萄糖的攝取和利用[2, 3];
-
作用於腸道,抑製腸壁細胞攝取葡萄糖,提高胰高血糖素樣肽- 1(GLP-1)水準[4, 5];
激活腺苷酸活化蛋白激酶(AMPK),改善肌肉、脂肪、肝臟的能量代謝[6-8]。
2單打獨鬥還是眾人抬柴?花式應用,卓群依舊
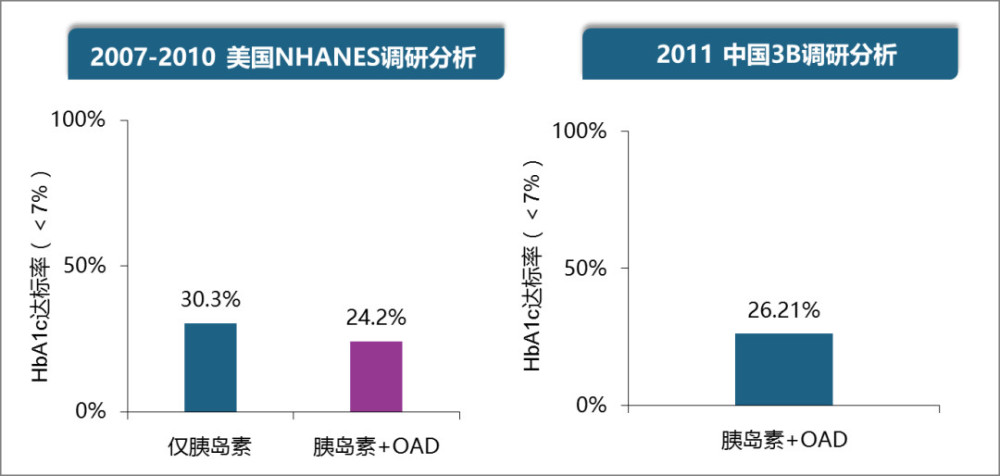
不論是單葯治療還是與其他口服降糖葯、胰島素聯合治療,二甲雙胍確切的降糖療效都已通過各類大型藥物研究的考驗,獲得共識推薦(表1)。下面對二甲雙胍單用/聯用以及部分特殊用法的具體療效逐一介紹。
表1:二甲雙胍的臨床療效


二甲雙胍單葯應用即效果卓群,29周可降低空腹血糖(FPG)3.2 mmol/L、餐後血糖(PPG)4.0 mmol/L、糖化血紅蛋白(HbA)1.8%(Ⅰ級) [9]。研究顯示基線HbA1c接近9%的新診斷患者,使用二甲雙胍單葯2000 mg可使近70%的患者達標。老將聯手,無往不利
除出類拔萃的單葯降糖療效,二甲雙胍可改善胰島素抵抗,減少肝糖輸出,增強肝臟和肌肉組織的胰島素敏感性,因此二甲雙胍可以與其他經典口服降糖藥物和胰島素聯合,可因作用機制互補或協同,產生1+1>2的效應。
中國的MERIT研究顯示,與胰島素單葯治療相比,二甲雙胍聯合胰島素可進一步降低HbA1c,減少胰島素用量、體重增加和低血糖風險;二者聯合與心血管疾病和腫瘤風險下降相關[10-15](Ⅰ級)。新老搭檔,一拍即合二甲雙胍不僅能與降糖老將聯手,與近年湧現的降糖新秀也配合默契:加用鈉-葡萄糖協同轉運蛋白2 (SGLT-2)抑製劑可在二甲雙胍療效的基礎上進一步改善血糖控制,顯著減輕體重及改善血壓[16-18]。除單用或與其他降糖藥物聯用於T2DM治療外,共識還針對二甲雙胍的3種特殊應用場景予以闡釋,即:接替短期胰島素強化治療、在1型糖尿病(T1DM)中的應用以及減重作用。
-
新診斷、初始HbA1c高的T2DM患者經短期胰島素治療後,接受以二甲雙胍為基礎的口服降糖葯治療與繼續應用胰島素治療的降糖療效相當 [19、20],以二甲雙胍為基礎的口服降糖葯治療能更好地改善β細胞功能和HbA1c水準(Ⅱ級),簡單易行、依從性好,較好地控制體重,成本-效益比更佳。
-
T1DM患者在胰島素治療基礎上加用二甲雙胍,能降低T1DM患者的胰島素用量、體重及血脂水準,且不增加低血糖及酮症酸中毒的發生風險(Ⅰ級)[21],尤其適用於胰島素劑量較大、體重增加明顯的患者(發生糖尿病酮症酸中毒、高血糖高滲綜合征、乳酸酸中毒患者禁用二甲雙胍)[22]。
二甲雙胍具有減輕體重的作用。基線BMI越高、腰圍越大的患者,使用二甲雙胍治療後體重下降越多[23, 24]。磺脲類、格列酮類和胰島素等藥物的使用可增加患者體重,聯合二甲雙胍可減輕上述藥物對體重增加的影響[18, 25](Ⅰ級)。
綜上,二甲雙胍豐富多樣的降糖機制為其發揮療效提供了有力保障。無論是單用還是與其他口服降糖葯/胰島素的靈活聯用,都可以個體化滿足不同患者對降糖、改善胰島功能、減重、降低低血糖風險等需求,切實提高糖尿病患者臨床獲益。
參考文獻
[1]Foretz M, Hebrard S, Leclerc J, et al. Metformin inhibits hepatic gluconeogenesis in mice independently of the LKB1/AMPK pathway via a decrease in hepatic energy state. The Journal of clinical investigation. 2010; 7: 2355-69.
[2]Sarabia V, Lam L, Burdett E, et al. Glucose transport in human skeletal muscle cells in culture. Stimulation by insulin and metformin. The Journal of clinical investigation. 1992; 4: 1386-95.
[3]Zhou G, Myers R, Li Y, et al. Role of AMP-activated protein kinase in mechanism of metformin action. The Journal of clinical investigation. 2001; 8: 1167-74.
[4]Forslund K, Hildebrand F, Nielsen T, et al. Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature. 2015; 7581: 262-266.
[5]Hur KY, Lee MS. Gut Microbiota and Metabolic Disorders. Diabetes & metabolism journal. 2015; 3: 198-203.
[6]Viollet B, Guigas B, Sanz Garcia N, et al. Cellular and molecular mechanisms of metformin: an overview. Clinical science. 2012; 6: 253-70.
[7]Foretz M, Guigas B, Bertrand L, et al. Metformin: from mechanisms of action to therapies. Cell metabolism. 2014; 6: 953-66.
[8]Coughlan KA, Valentine RJ, Ruderman NB, et al. AMPK activation: a therapeutic target for type 2 diabetes? Diabetes, metabolic syndrome and obesity : targets and therapy. 2014: 241-53.
[9]DeFronzo RA, Goodman AM. Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. The Multicenter Metformin Study Group. The New England journal of medicine. 1995; 9: 541-9.
[10]Hemmingsen B, Christensen LL, Wetterslev J, et al. Comparison of metformin and insulin versus insulin alone for type 2 diabetes: systematic review of randomised clinical trials with meta-analyses and trial sequential analyses. Bmj. 2012: e1771
[11]Strowig SM, Aviles-Santa ML, Raskin P. Comparison of insulin monotherapy and combination therapy with insulin and metformin or insulin and troglitazone in type 2 diabetes. Diabetes care. 2002; 10: 1691-8.
[12]Kooy A, de Jager J, Lehert P, et al. Long-term effects of metformin on metabolism and microvascular and macrovascular disease in patients with type 2 diabetes mellitus. Archives of internal medicine. 2009; 6: 616-25.
[13]Guo L, Chen L, Chang B, et al. A randomized, open-label, multicentre, parallel-controlled study comparing the efficacy and safety of biphasic insulin aspart 30 plus metformin with biphasic insulin aspart 30 monotherapy for type 2 diabetes patients inadequately controlled with oral antidiabetic drugs: The merit study. Diabetes, obesity & metabolism. 2018; 12: 2740-2747.
[14]Liao L, Yang M, Qiu LL, et al. Appropriate insulin initiation dosage for insulin-naive type 2 diabetes outpatients receiving insulin monotherapy or in combination with metformin and/or pioglitazone. Chinese medical journal. 2010; 24: 3684-8.
[15]Giugliano D, Quatraro A, Consoli G, et al. Metformin for obese, insulin-treated diabetic patients: improvement in glycaemic control and reduction of metabolic risk factors. European journal of clinical pharmacology. 1993; 2: 107-12.
[16]Lavalle-Gonzalez FJ, Januszewicz A, Davidson J, et al. Efficacy and safety of canagliflozin compared with placebo and sitagliptin in patients with type 2 diabetes on background metformin monotherapy: a randomised trial. Diabetologia. 2013; 12: 2582-92.
[17]Yang W, Han P, Min KW, et al. Efficacy and safety of dapagliflozin in Asian patients with type 2 diabetes after metformin failure: A randomized controlled trial. Journal of diabetes. 2016; 6: 796-808.
[18]Yang T, Lu M, Ma L, et al. Efficacy and tolerability of canagliflozin as add-on to metformin in the treatment of type 2 diabetes mellitus: a meta-analysis. European journal of clinical pharmacology. 2015; 11: 1325-32.
[19]Cheng Q, Yang S, Zhao C, et al. Efficacy of metformin-based oral antidiabetic drugs is not inferior to insulin glargine in newly diagnosed type 2 diabetic patients with severe hyperglycemia after short-term intensive insulin therapy. Journal of diabetes. 2015; 2: 182-91.
[20]Retnakaran R, Choi H, Ye C, et al. Two-year trial of intermittent insulin therapy vs metformin for the preservation of beta-cell function after initial short-term intensive insulin induction in early type 2 diabetes. Diabetes, obesity & metabolism. 2018; 6: 1399-1407.
[21]Liu C, Wu D, Zheng X, et al. Efficacy and safety of metformin for patients with type 1 diabetes mellitus: a meta-analysis. Diabetes technology & therapeutics. 2015; 2: 142-8.
[22]Lund SS, Tarnow L, Astrup AS, et al. Effect of adjunct metformin treatment on levels of plasma lipids in patients with type 1 diabetes. Diabetes, obesity & metabolism. 2009; 10: 966-77.
[23]Ji L, Li H, Guo X, et al. Impact of baseline BMI on glycemic control and weight change with metformin monotherapy in Chinese type 2 diabetes patients: phase IV open-label trial. PloS one. 2013; 2: e57222.
[24]Zhou L, Cai X, Yang W, et al. The magnitude of weight loss induced by metformin is independently associated with BMI at baseline in newly diagnosed type 2 diabetes: Post-hoc analysis from data of a phase IV open-labeled trial. Advances in clinical and experimental medicine : official organ Wroclaw Medical University. 2017; 4: 671-677.
[25]Charbonnel B, Schernthaner G, Brunetti P, et al. Long-term efficacy and tolerability of add-on pioglitazone therapy to failing monotherapy compared with addition of gliclazide or metformin in patients with type 2 diabetes. Diabetologia. 2005; 6: 1093-104.












TAG: |